Surgeons' Working Environment
Introduction and Background
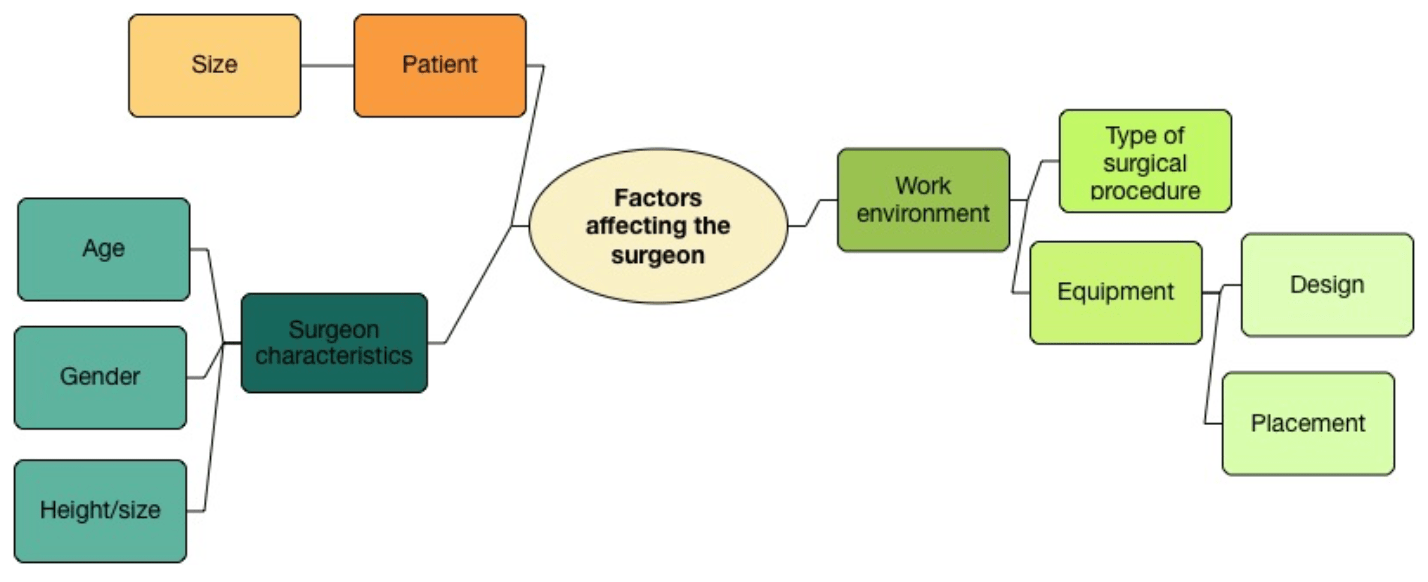
Medicine is a sector designed to provide healing and health for individuals whom partake in it, yet surgeons often suffer while providing care. Poorly designed operating equipment and postures maintained while performing surgical procedures can at minimum lead to discomfort or at worst case force a surgeon into retirement from injuries.
As the human population increases in size, there are increased prevalences of gynecological disorders. Because of this, surgeons are having to operate on larger patients. There is an abundance of research on obesity causing an increase of issues with patients, but little research on how larger patient sizes affect the surgeon. Particularly research that considers surgical port placement and patient sizes on posture.
The Objective
To evaluate the physical fit of the workplace to surgeons during gynecological minimal access surgery, including bariatric patients.
The study objectives included:
- Understanding the range of surgeon’s body sizes that are accommodated at the surgery workstation;
- Assessing work-related risk; and
- Exploring the effects of variables of surgical port positions and patient size on posture.
The Approach
The research process began with a systematic literature review to gain knowledge of gynecological surgery as well as define aims and objectives. Observation of live surgeries, measurement of operating room equipment, and further research aided in the development of the methods for data collection.

Due to the nature of real world research, the surgical environment and the limited time to complete the study, data was unable to be collected during actual surgical procedures. Therefore observations were conducted in a pseudo-realistic environment, where the operating room and surgery could be simulated. Two simulated abdomens were used to represent both 50th and 99.99th percentile adult female.
The study focused on quantitative methods of data collection and analysis, including observational, anthropometric and postural analyses data. Five anthropometric dimensions were collected from participants (stature, elbow height, wall-acromion distance and shoulder biacromial breadth). Postures were analyzed using Rapid Entire Body Assessment (REBA).
Qualitative data was collected separately and later synthesized together here.
The Observations
Observation was a crucial part of this study as it was beneficial in establishing mismatches between an individual and their working environment.
Participants were asked to set up the surgical table, placement of laparoscopic monitors and working port placements to mimic their positioning preference in the operating room. The following postures were captured of the participants on both the 50th percentile abdomen and the 99.99th percentile abdomen:
- surgeon port choice – most frequent posture;
- surgeon port choice – most extreme posture;
- bilateral port placement;
- midline port placement;
- unilateral port placement

The Analysis
REBA was used for coding postures from photographs taken during observations and then given action scores to determine the musculoskeletal risk.
Relationship between the working posture and variables including working height, patient size and port position were explored. Working heights for the operating room table in consideration to patient abdominal height were established.
The Results
Work Surface Height
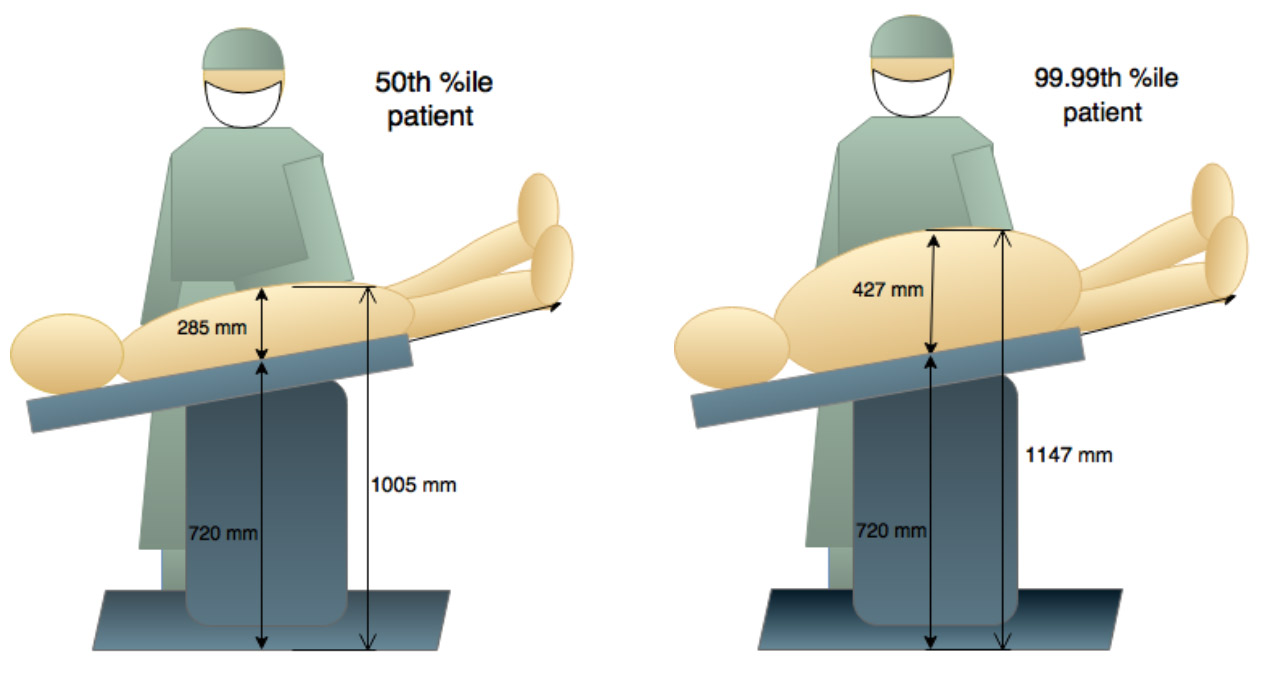
The minimum table height (Eschmann T20-m) measured 1005mm for the 50th %ile and 1147mm for the 99.99th %ile abdomen. The figure below illustrates the working heights with these prospective patients and a surgeon with an elbow height around 995 mm (41st %ile for a female or 4th %ile male). The figure indicates the minimum height of the surgical table is problematic for surgeons of shorter stature. This height of table would cause strain on this surgeon as they would have to raise their upper limbs.
Postural Analyses
The resulting action levels scored from REBA analysis ranged between a low risk level (1) to a high risk level (3), with no postures scoring in action levels 0 or 4. The action levels were then separated into two categories: satisfactory and unsatisfactory. Satisfactory postures were those with an action level of 1, as they did not necessarily require further action. While satisfactory postures are not without risk, they were the most acceptable posture seen during observations. Unsatisfactory postures were those coded with the action levels of 2 or 3, due to the necessity of required action.
| Port Positions | Action Level 1 | Action Level 2 | Action Level 3 | Percentage Unsatisfactory Action Level |
|---|---|---|---|---|
| Bilateral 50 | 1 | 4 | 6 | 91 |
| Bilateral 99 | 0 | 7 | 4 | 100 |
| Midline 50 | 0 | 11 | 0 | 100 |
| Midline 50 | 2 | 6 | 3 | 82 |
| Unilateral 50 | 8 | 2 | 0 | 20 |
| Unilateral 99 | 6 | 5 | 0 | 45 |
Action level frequencies with port position postures
| Surgeon Port Choice | Action Level 1 | Action Level 2 | Action Level 3 | Percentage Unsatisfactory Action Level |
|---|---|---|---|---|
| Most frequent 50 | 2 | 6 | 2 | 73 |
| Most frequent 99 | 6 | 5 | 0 | 45 |
| Most extreme 50 | 0 | 4 | 7 | 100 |
| Most extreme 50 | 0 | 4 | 7 | 100 |
Action level frequencies of frequent and extreme postures
Discussion
Human variability must be accounted for in the dimensions of the surgeon’s workstation, as a mismatch between their measurements and the users will result in suboptimal working postures placing the surgeon at risk for musculoskeletal injury.
While data regarding larger patient abdominal height causing more risk to the surgeon were not significant from postural analysis, anthropometric data indicates there is an issue, simply by the fact that as patient abdominal height increases the working height also increases. This increase excludes more of the surgeon population from an optimum working height.
Surgeon’s port placement and chosen working ports throughout the surgery also provide evidence of influencing the surgeon’s working posture as different port positions change the working height, indicating that there is a variable working height. Unilateral port placement, during hysterectomy surgery as observation and postural analyses data has established, involves less risk.
Further investigation into port positions, patient abdominal height and working postures should be explored to validate the findings in this study and better understand the influence theses variables have on working posture.
